A Natural Alternative to Statins

If you have high cholesterol, you’ve likely been urged by your doctor to start taking statins, or at least cautioned that they will be prescribed if your cholesterol increases any more. This is no surprise, as statins are the go-to drug that most physicians rely on to lower cholesterol. Statins do indeed lower cholesterol for most people, and high cholesterol can be dangerous, increasing the risk of atherosclerosis, which in turn increases the risk of heart disease, heart attack, and stroke. Statins have no doubt helped millions of people, but sometimes at a price.
Doctors are sometimes quick to prescribe statins even when there is a low to moderate risk of cardiovascular risk, taking a “better safe than sorry approach”. The problem is that many people have at least some sort of side effect from statins, ranging from dizziness and muscle pain to increased blood sugar and neurological problems like sexual dysfunction and memory loss. Aside from the real damage this may cause, the psychological impact that this may have on someone with a low to moderate risk of cardiovascular problems may cause them to give up statins altogether and resist using them again even if their cardiovascular risk increases.
Statins are probably prescribed too often, and without considering more natural interventions like exercise, modifying the diet, and supplementing with omega-3 fatty acids from fish oil (see our discussion of how important omega-3s can be). In fact:
“The current American College of Cardiology guidelines for statin use emphasize collaborative decision-making between providers and patients,” Tomas Ayala, MD, FAAC, a cardiologist at Mercy Medical Center in Baltimore, Maryland, told Healthline.“In general, statins are not recommended for low-risk patients. For patients at high risk… statins are recommended for primary prevention of cardiac events. For those of immediate risk, statins are recommended only if the patient also has a high-risk illness, such as diabetes, peripheral vascular disease, or cerebrovascular disease.” (Tony Hicks, Healthline, Oct 19, 2019).
So current standards are to consult with the patient and they are not recommended for low-risk patients. Does this sound like your last consult on the subject with your physician? Likely not. Many physicians order their patients to take statins and may be unlikely to discuss side effects or alternatives. In addition, there is some question about how much cholesterol is to blame for eventual cardiac events:
“A new national study has shown that nearly 75 percent of patients hospitalized for a heart attack had cholesterol levels that would indicate they were not at high risk for a cardiovascular event, based on current national cholesterol guidelines.” (Science Daily, Jan 13, 2009)
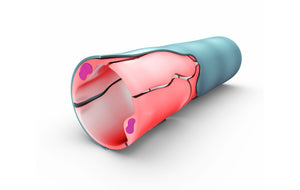
The same study, out of UCLA did point out that very high levels of cholesterol still correlated with heart attacks, but did not control for other things that can also contribute. The point is that other factors can be equally as important, if not more important than cholesterol. A good example is oxidized LDL. Oxidized LDL cholesterol is made in the body when low-density lipoprotein (LDL), sometimes called “bad” cholesterol, goes through a chemical reaction with free radicals (unstable molecules made during normal cell metabolism). Oxidized LDL cholesterol can cause inflammation in the arteries, leading to the formation of plaques. Over time, fat, cholesterol, and other substances build up in the walls of the arteries, causing the plaques to grow. Plaque buildup can partially or completely block blood flow within an artery, increasing a person’s risk for coronary heart disease, peripheral vascular disease, cerebrovascular disease, stroke, and heart attack.
Why is oxidized LDL relevant to the discussion over the effectiveness of statins? First, because oxidized LDL is likely a better predictor of cardiac events than just cholesterol (see this study for instance), and second because statins can decrease levels of coenzyme Q10 in the body (Qu H, et al, European Journal of medical research. 2018). CoQ10 is fundamental to the production of cellular energy in the mitochondria and is a powerful antioxidant. Its ability to destroy free radicals means that your CoQ10 levels can have a profound effect on your cardiac health. This means that for some people, not only might they have a lesser risk for heart attack or stroke, but if they are prescribed statins, their risk factors may actually go up.
Again, statins may be essential for some people, but they are probably overprescribed, can cause side effects (some quite severe), and should be reserved for those with higher cholesterol levels. They also shouldn’t be the front-line defense against cholesterol (or more accurately, cardiac health). A more mediated, reasonable, and natural approach should be tried first, consisting of shifting to a more heart-healthy diet (the Mediterranean diet is a good example), introducing or improving your exercise regime, taking at least a daily dose of omega-3 fatty acids from fish oil, and introducing other botanical supplements that lower cholesterol and improve other aspects of cardiac risk factors. An excellent candidate for the latter is bergamot.
Bergamot is a citrus fruit that contains flavonoids and polyphenols that can bind with an enzyme involved in cholesterol production. Studies have shown that bergamot may help to lower total cholesterol and LDL cholesterol, which can build up in the arteries and cause plaque. Bergamot may also help to increase HDL cholesterol, which can escort cholesterol out of the arteries to the liver and protect arterial health. Bergamot may be an effective supplement to cholesterol drugs or a natural alternative to statin drugs, which cannot raise HDL cholesterol.
Bergamot has been used for centuries in traditional medicine in Calabria, Italy, where it grows to treat inflammation, fever, and other ailments. It’s used extensively in the flavoring, perfume, and cosmetics industries because of its pleasant scent and over 100 different volatile compounds. Many citruses contain flavonoids and can possibly have a beneficial effect on cardiac health, but bergamot has an especially high number of them. Given its long-time use, bergamot has proven to be safe, and its high number of volatile compounds and flavonoids, it’s a better candidate than other citrus fruits for this role. Unlike other citruses, bergamot is not eaten as a fruit since it is mostly rind. Bergamot oils and dried peel have traditionally been used (it is the extra flavor in Earl Grey tea), but it can also be juiced. Although you are likely to get some benefit from those forms, it is far more potent as a supplement and composed of a reasonable percentage of a polyphenolic fraction of bergamot, which is what the research supports. Progressive Nutracare carries its own version of this product. A comprehensive review of the scientific literature has found evidence of several mechanisms whereby bergamot can assist in lowering cardiac risks:
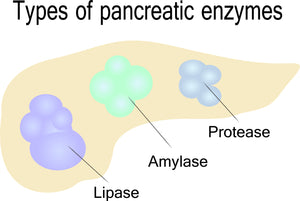
“Multiple clinical trials have provided evidence that different forms of orally administered bergamot can reduce total cholesterol and low-density lipoprotein cholesterol. In vitro mechanistic studies have provided evidence that polyphenols from the bergamot can alter the function of AMPK and pancreatic cholesterol ester hydrolase (pCEH). The use of bergamot in multiple clinical trials has consistently shown that it is well tolerated in studies ranging from 30 days to 12 weeks.” (Nauman MC, Johnson JJ. Clinical application of bergamot [Citrus bergamia] for reducing high cholesterol and cardiovascular disease markers. Integr Food Nutr Metab. 2019 Mar.)
“Citrus fruits are rich in flavonoids and have long been associated with improving human health outcomes in areas that include improved immune response, coronary artery disease, heart failure, and high cholesterol. One citrus fruit in particular that has gained attention for improving health outcomes is the bergamot (Citrus bergamia)” (Same source cited above)
Aside from lowering cholesterol, and generally contributing to cardiac health, bergamot has specifically been found to be effective in lowering oxidized LDL:
“Oxidation of low-density lipoprotein particles is a harmful form of cholesterol that results from free radical damage. This form of oxidative damage, along with increased inflammatory events, has been associated with atherosclerosis that ultimately alters cardiovascular blood flow. Several constituents including naringin, neoeriocitrin, and rutin from the bergamot have been reported to lower the oxidation of LDL particles.” (same source cited above)
Overall, bergamot seems an excellent candidate to try along with fish oils, and changes in diet and exercise instead of statins if your cholesterol levels are low or moderate, or if you can’t tolerate statins. If your cholesterol levels are higher, and you are already taking statins, adding those same regimens plus fish oils and bergamot may still make a difference, and perhaps allow you to eventually leave statins behind:
“The results of five different clinical trials using bergamot in various forms suggest the polyphenol fraction can lower LDL-C and total cholesterol. Several studies suggested that bergamot polyphenols can reduce triglycerides and increase HDL-C ……Three of the studies suggested an increase in HDL by up to 4 mg/dl (Table 1). This is significant because HDL is often difficult to increase apart from lifestyle changes. …….Taken together, these early clinical trials along with the mechanistic studies that have been performed suggest that bergamot can reduce total cholesterol and LDL-C through mechanisms that are distinct from current pharmaceutical approaches.” (same source cited above).
- Tags: Article Cardiovascular
- Robert Thomas





Comments 0