Natural Alternatives to Antibiotics, and Why You Should Care.

Antibiotics can save your life when you need them. Their invention and rapid adoption were among the great triumphs of public health. Bacterial infections that once might have easily led to sepsis and death can be reversed within a week or ten days. Conditions that could cause a lifetime of malingering conditions until the end, like syphilis, can be cured with courses of antibiotics. There is no denying their worth and necessity at times, but antibiotics have a dark side as well.
Partially because of the belief by some people that they are cure-alls, some patients will demand antibiotics for conditions that don’t warrant them. Antibiotics should really be called “antibacterials”, for that is what they target. They don’t kill viruses, nor most classes of fungi, and they provide no treatment for conditions that stem from them. When someone has a sore throat, stopped-up sinuses, or a lingering cough, they may demand a prescription for antibiotics from their doctor because they believe they’ll be cured, or “just in case” it’s a bacterial infection. Many doctors give in they either don’t want to fight with the patient or buy the “just in case” argument, even without any confirmatory testing of whether the condition is bacterial. In fact, doctors will often prescribe antibiotics prophylactically when you “might” have a bacterial infection, or when a wound you have that isn’t infected has the possibility of becoming so.
So what’s wrong with this? If antibiotics are so effective, then if it turns out that you have a bacterial condition it will cure it, right? If not, no harm no foul. Unfortunately, this isn’t true and there are dangers that come with antibiotics use. The first is that antibiotics are overused. Aside from human use, they are used in most livestock, poultry, and farmed salmon, and antibiotic runoff from feedlots, chicken holding pens, and fish farms pollute our waterways and can be found in our drinking water. “A study released in 2010 by the U.S. Geologic Survey, for example, found that a variety of antibiotics -- azithromycin, sulfamethoxazole, and ciprofloxacin, among others -- were detected in 11 of 12 sampling sites in Ohio [source: Finnegan et al.].” Similar studies in other states show antibiotics in our waters- even in rural areas. “But researchers worry that drinking water with trace levels of drugs may cause a gradual buildup inside your body that might be harmful [source: Harvard Health Letter].”
Again, should this concern us? The reason that it should is that overuse of antibiotics, and issues like antibiotic pollution, cause the bacteria that are being targeted in the course of justified antibiotic treatment to become resistant to the specific drug being used, and sometimes to that whole class of antibiotics. When this happens, stronger and potentially more dangerous antibiotics are required for treatment. This bacterial resistance to antibiotics could potentially come from the buildup of low levels of antibiotics in our bodies. Another way is that the bacteria themselves are exposed to antibiotic pollution in our waterways and evolve to become resistant to those antibiotics in the wild. The CDC says that: “antibiotic resistance is found in one of the most basic resources for life – water. Antibiotic-resistant pathogens and their genes have been found in streams, rivers, lakes, and oceans. They can often be traced back to discharge flowing from hospitals, farms, or sewage systems. Even properly functioning wastewater treatment systems may not fully remove resistant pathogens and their genes.” This problem can snowball in nature: “Antibiotic-resistant pathogens can also share their resistance genes with other pathogens. Even if they have never been exposed to antibiotics, this allows the other pathogens to become resistant to antibiotics.” (CDC, again).
This problem of antibiotic-resistant pathogens can be caused in an even simpler way. Misuse of the antibiotic by a patient. The reason that it is so important to finish an entire course of antibiotics rather than stop merely when you start to feel better, is that you might not have completely killed off the bacteria at the root cause of your condition. If you’ve killed 90% of the bacteria, you may feel better, but stopping the delivery of the antibiotic to your system may mean that the other 10% are able to survive- with an enhanced ability to resist that antibiotic in the future. The result could be that your infection comes roaring back with the antibiotic-resistant strain of bacteria that now requires a more powerful drug to kill it, or if not, you may shed that strain of antibiotic-resistant bacteria into the wild.
The impact of resistant strains of bacteria isn’t just that you have to take another round of a stronger antibiotic, it’s that those stronger strains need to be reserved for more severe infections that other patients (or yourself one day) may have. These resistant strains of bacteria are increasing at an accelerating rate, and the worry is that they’ll eventually evolve to the point that no class of antibiotic at all will work against them. These bacteria are called pan-resistant bacteria1. They are resistant to all antibiotics available for treatment and can cause severe infections that are difficult to treat1. The impact of resistant bacteria can be devastating according to the CDC: “Antimicrobial resistance is an urgent global public health threat, killing at least 1.27 million people worldwide and associated with nearly 5 million deaths in 2019. In the U.S., more than 2.8 million antimicrobial-resistant infections occur each year. More than 35,000 people die as a result, according to CDC’s 2019 Antibiotic Resistance (AR) Threats Report. When Clostridium difficile—a bacterium that is not typically resistant but can cause deadly diarrhea and is associated with antimicrobial use—is added to these, the U.S. toll of all the threats in the report exceeds 3 million infections and 48,000 deaths.”
Aside from the impact on public health as a whole, there are potential dangers to yourself and others just from having to take a stronger antibiotic that can treat the antibiotic-resistant strain of bacteria:
“Bacteria and fungi do not have to be resistant to every antibiotic or antifungal to be dangerous. Resistance to even one antibiotic can mean serious problems. For example:
“Antimicrobial-resistant infections that require the use of second- and third-line treatments can harm patients by causing serious side effects, such as organ failure, and prolong care and recovery, sometimes for months
- Many medical advances are dependent on the ability to fight infections using antibiotics, including joint replacements, organ transplants, cancer therapy, and the treatment of chronic diseases like diabetes, asthma, and rheumatoid arthritis
- In some cases, these infections have no treatment options
- If antibiotics and antifungals lose their effectiveness, then we lose the ability to treat infections and control these public health threats.”
Choose to help protect public health (and eventually your own) by limiting your use of antibiotics.
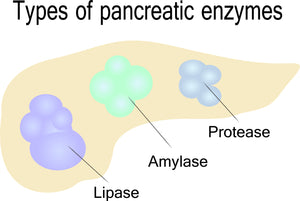
Aside from the impact on public health, antibiotic use can cause harm to your own body as well. Even if you take antibiotics as directed, and even if you never encounter a drug-resistant strain of bacteria, antibiotic use can impact you- particularly if you frequently take them. Just one course of antibiotics can be like a bomb going off in your gut. Antibiotics devastate your microbiome, massively reducing beneficial strains of flora that are necessary for proper gut function, and allowing harmful flora to proliferate. This harmful flora is more likely to cause gut dysbiosis, inflammation both in the gut and elsewhere in the body, and cause malabsorption of nutrients. Avoiding antibiotics whenever possible, and being sure you need them before taking them are the best bets to avoid these harms, but it’s also why you should always take a probiotic along with antibiotics. People who take multiple courses of antibiotics are more likely to have even more gut damage, be more likely to need more powerful strains in the future, and perhaps more likely to generate antibiotic-resistant strains.
Another way that your body can be harmed by antibiotics is by your doctor giving you a class of antibiotics that causes severe side effects, often worse than the initial infection. This is, of course, a possibility as the strength of an antibiotic has to be escalated in the face of a resistant strain of bacteria, but can also be because your doctor gives you a class of antibiotic that is too strong for what you need, or that you react to an antibiotic. There are classes of antibiotics that have black box warnings on them that are still being prescribed by some doctors. A good example are fluoroquinolones. Fluoroquinolones are a family of broad-spectrum, systemic antibacterial agents that have been used widely as therapy for respiratory and urinary tract infections. Epidemiological studies have reported an increased risk of rare adverse effects associated with fluoroquinolones including tendinopathy and tendon rupture, peripheral neuropathy, and aortic aneurysm.
Antibiotics in general can cause side effects such as diarrhea, nausea, vomiting, rash, upset stomach, sensitivity to sunlight, and fungal infections of the mouth, digestive tract, and vagina. Most adverse events related to antimicrobials are reversible rapidly on cessation of the medication. Irreversible toxicities include aminoglycoside-induced ototoxicity, Stevens-Johnson syndrome, and toxicity secondary to nitrofurantoin. Whew! That’s a lot to consider, huh?
So when can you avoid antibiotics, and is there anything you can take instead? To start with, don’t take antibiotics for anything but a bacterial infection. Not only will they not work, but you’ll potentially be harming yourself and others for absolutely no reason. Secondly, if you have a minor bacterial infection that is or may resolve on its own, you can probably safely avoid antibiotics. Get the advice of your doctor and be your own advocate. Tell them you want to avoid antibiotics unless absolutely necessary. Third, avoid repeated courses of antibiotics if you can. If you get frequent sinus infections, for instance, try lavages, sprays, and neti-pots rather than yet another course of antibiotics (your gut, and the rest of your body, will thank you).
To help you when you have a more minor bacterial infection, consider a product that contains natural ingredients that have been shown to have antibacterial properties. Some natural ingredients that have research to this effect include olive leaf extract, neem leaf, sweet wormwood, berberine, oregano, thyme, barberry, and black walnut. Parabiotic Plus includes all of these ingredients if you’d like to try a natural approach. Other natural possibilities that also have some research are bilberries, grape seed extract, shiitake mushroom extract, goldenseal, noni fruit, garlic, milk thistle, echinacea, galbanum, tea tree oil, and gentian. All of these ingredients can be found in Biocidin Liquid. Both Biocidin and Parabiotic Plus are available from the Nutracare store. Limit your drug use of antibiotics, saving them for truly crucial times- both for your and the world’s benefit.
- Tags: Article Gastrointestinal
- Robert Thomas





Comments 0